Canadian doctors are using 'outdated' guidelines to screen for cancer, experts warn
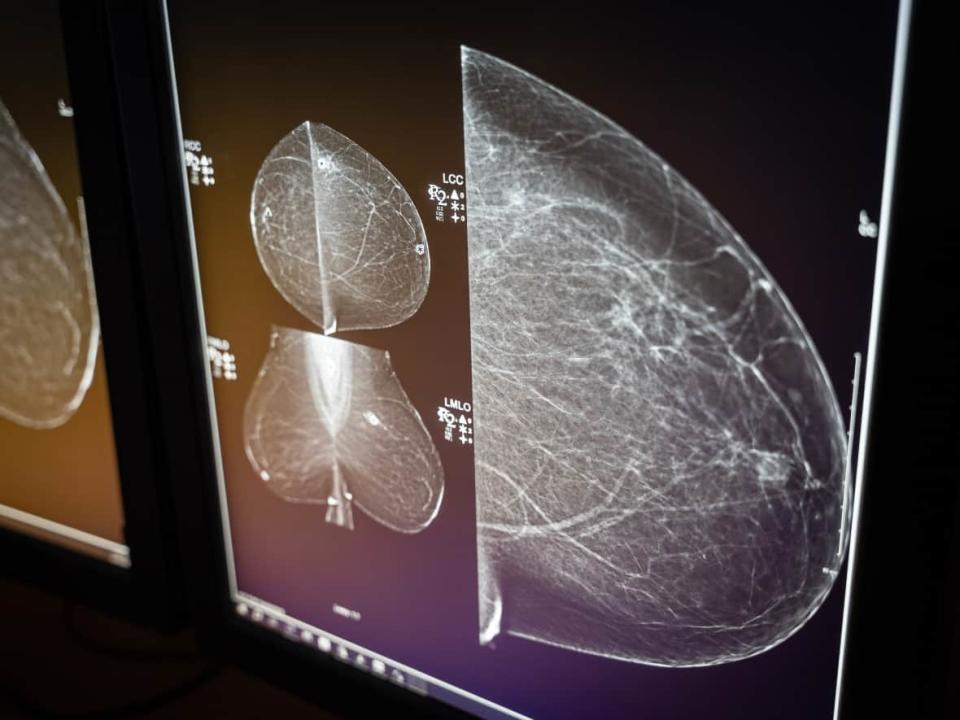
Carolyn Holland can't help wondering how many years of her life she's lost because her breast cancer was diagnosed late.
The Ottawa mom first discovered lumps in her breasts while in the shower. At 43 years old, she'd never had a mammogram.
After seeing her doctor, she was sent for a scan, which confirmed the cancer. But at that point it had already advanced. Holland needed two types of chemotherapy, radiation, the removal of her lymph nodes and a double mastectomy.
"This shouldn't happen to other women. It's preventable," Holland said.
Holland's doctors told her that her treatment could have been less drastic had the cancer been detected sooner. But Canada's national guidelines do not recommend routine breast cancer screening for women under the age of 50.
"Had I been able to access screening at 40, this wouldn't have been my outcome," she said.

A group of medical experts say Canadian lives are at risk because family doctors are using outdated guidelines to decide whether, and when, to send their patients for routine cancer screenings.
The guidelines are issued by the Canadian Task Force on Preventive Health Care, an arms-length panel of 15 doctors and other primary care providers set up by the federal government. The independent volunteer panel examines the research on screening and preventing various illnesses, including cancer.
"These guidelines impact millions of Canadians. The consequences are grim. Current task force guidelines often limit access to critical life-saving screening," said Dr. Shiela Appavoo, an Edmonton-based radiologist.
She's with the Coalition for Responsible Healthcare Guidelines, a group of cancer specialists, family doctors and patients calling for changes to how the guidelines are created.
The coalition says the task force is using outdated research, doesn't properly take in the advice of experts and is far too slow to update its recommendations.
Family doctors taught to follow national guidelines
The task force's breast cancer screening guidelines are set to be updated next month. The current recommendations, last updated in 2018, recommend against broad screening of women in their 40s.
The Canadian Cancer Society withdrew its support for the guidelines in December 2022, citing concerns that they were not keeping pace with new research, in particular the growing incidence of cancer in younger populations around the world. The latest statistics show the cancer most commonly diagnosed in Canadians aged 30 to 49 is breast cancer.
Many provinces have ignored the task force guidelines by lowering the age when they offer breast cancer screening to include women in their 40s.
WATCH | Cancer screening guidelines are out of date, experts say:
British Columbia, Nova Scotia, P.E.I. and Yukon all allow women to access a mammogram in their 40s. Alberta and the Northwest Territories start screenings at 45. Ontario will start covering mammograms for women in their 40s this fall.
While some provinces have expanded screening eligibility to younger women, many doctors still might not send their patients for the test because the national guidelines recommend against it, Appavoo said.
"Unfortunately, a lot of family physicians are taught and trained to follow the task force guidelines," Appavoo said.
That's a problem, she said, because a patient is most likely to go for cancer screening if their doctor recommends it.
"So it is really important to give family doctors appropriate and adequate information on who to screen and when to screen," Appavoo said.
The lack of leadership on national guidelines has also led to piecemeal coverage across the country, she said, because some Canadians have access to cancer screening sooner than others.
Cancer research from 1960s still being used
Dr. Anna Wilkinson saw firsthand the impact of those guidelines she was taught to follow. As an Ottawa family physician who treats oncology patients, she's worked with many women in their 40s dying of breast cancer.
"They asked for a mammogram and they were told, 'No, you don't need one because you're in your 40s,'" Wilkinson said. "It's heartbreaking."
That prompted Wilkinson to co-author a study that compared breast cancer statistics from provinces that screened women in their 40s to stats from provinces that followed the task force guidelines. Her study found that earlier screening led to significantly improved survival rates.
Despite new evidence from Canada and around the world about the benefits of screening women at younger ages, Wilkinson said the task force continues to weigh outdated data when making its recommendations.
The task force is still using data from a 1963 trial to determine whether women should be screened today, she said.
"That is completely irrelevant at this point," Wilkinson said. "There is nothing about the way that breast cancer screening was done or treatment was done in the 60s that reflects today's practices."
Other cancer guidelines out of date, experts say
The task force screening guidelines for several other types of cancer also lag behind what many experts, cancer organizations and other jurisdictions recommend.
"They are harming Canadians because they are leading us to diagnose cancers at a later stage when we know survival is worse and when the costs of treatment are more," Wilkinson said.
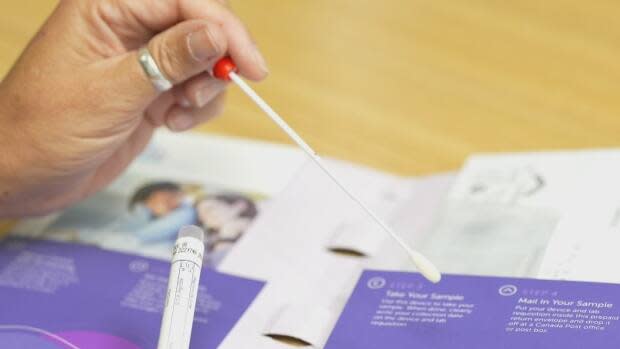
The guidelines for cervical cancer haven't been updated since 2013 and aren't due to be revisited until 2025.
The task force currently recommends against screening for HPV, citing concerns the research is too premature. HPV is the virus that causes most cases of cervical cancer and it can be detected much sooner than a Pap test detects changes in cervical cells.
By comparison, the U.K.'s screening advisory body began recommending HPV screening in 2016 while Australia replaced routine Pap tests with HPV screening in 2017. Many provinces have begun screening for HPV, despite the national guidelines.
The task force's guidelines for lung cancer screening were last updated in 2016 and are not due to be updated until 2026. The task force gives what it calls a "weak" recommendation to screen heavy tobacco users with low-dose CT scans, despite research that has found CT scans help to detect lung cancer early and decrease the number of deaths.
The Canadian Cancer Society recommends that heavy smokers between 55 and 74 be screened every three years.
"Half of the time when we diagnose people with lung cancer, it's already Stage 4, which is incurable," said Dr. Paul Wheatley-Price, who leads the lung cancer program at the Ottawa Hospital Cancer Care Centre.
He said the amount of time it takes the task force to update its guidelines is "baffling."
The task force's guidelines on prostate cancer, which won't be updated until 2026, recommend against prostate specific antigen (PSA) blood tests. The Canadian Urological Association has criticized that advice since it was issued in 2014; it argues that trials show screening reduces prostate cancer deaths by up to 44 per cent.
"Those (task force) guidelines are about 10 years old and we've made a huge amount of progress," said Dr. Fred Saad, director of prostate cancer research at the Montreal Cancer Institute. "The input that came from experts was basically ignored."
The Canadian Cancer Society also recommends that men consider having a PSA test done starting at age 50, and that Black men begin testing at 45.
The task force also doesn't offer different guidelines for screening based on a patient's ethnicity, despite research that shows some populations are diagnosed with certain cancers at earlier ages. Inuit, for example, are more than twice as likely as the rest of the population to be diagnosed with lung cancer, according to the Canadian Partnership Against Cancer.
The risk of 'over-diagnosis'
New studies are coming out all the time, said task force member Dr. Eddy Lang — but they don't always offer enough evidence for the panel to change its recommendations.
"Our system is arguably in crisis and it may not be the best use of resources to be detecting things early," Lang said, who works as an emergency room physician in Calgary.
While the task force does consult with cancer experts, Lang said, those experts don't get to set the guidelines — and there's a good reason for that.

"Someone who's been researching and advocating in the breast cancer or prostate cancer field for their whole career might have a different view than a neutral group that is trying to make recommendations for family doctors," he said.
"Experts in the area will often focus a bit more on the benefits of screening and may not have as much attuned understanding or awareness of the harms that [are] often seen more at the primary care level, and that is our audience."
Lang said the task force needs to factor in the risks associated with over-diagnosis — of subjecting patients to cancer treatments that can be more harmful than the cancer itself, or of treating a cancer that never would have caused a problem in the first place.
"I thought it was common knowledge, you screened for cancer, you catch it early, you nip it in the bud. But when I joined the task force and started looking at the evidence, I was actually blown away at how significant the harms can be of early detection," he said.
But cancer survivor Carolyn Holland said Canadians have the right to know if they have cancer, and then make informed decisions about treatment.
"What I would tell the task force is, you are not saving us from harm," she said. "You're actually putting us in harm's way by denying us screening, by denying us the chance to catch cancers early."
 Yahoo Sports
Yahoo Sports 